

Patients were included after informed consent and oral approval. Patients with periprosthetic acetabular fractures were included as well, provided that they received a medial buttress as part of ORIF (group 2). Only patients with a medial buttress were included in our study (group 1). Flowchart of excluded and included patients. In this study, we analysed the efficacy of the concept of medial buttressing in ORIF of geriatric acetabular fractures or periprosthetic acetabular fractures. There are only a few studies with limited follow-up and there are no recommendations available. Until today, there is a lack of knowledge about optimal treatment of fractures of the acetabulum in patients of higher age. Both enable a direct exposure of the lower part of the anterior column and the quadrilateral surface. The modified Stoppa and the pararectus approach are intrapelvic approaches, which have been developed more recently. Optimal indications for this approach are anterior wall, anterior column, anterior wall or column with posterior hemi-transverse and both column fracture. Letournel developed the ilioinguinal approach for open reduction and internal fixation of acetabular fractures with involvement of the anterior column and quadrilateral plate. The insertion of an additional or specific implant at the inner side of the reduced quadrilateral surface may be a good solution in counteracting the supero-medial forces to the hip joint and preventing secondary protrusion of the femoral head or loosening of the acetabular cup. In this intervention, ORIF has the primary goal of creating a stable socket for cup placement. ORIF of the acetabular fracture is rarely combined with primary THA. But there is an enhanced risk of symptomatic or asymptomatic cup loosening in THA after acetabular fracture. An alternative treatment is primary total hip arthroplasty (THA). The goal is achieving an anatomical reduction and stable fixation of the acetabulum to prevent secondary osteoarthritis of the hip joint. Open reduction and internal fixation (ORIF) of acetabular fractures in patients of old age is an accepted method of treatment. The quadrilateral surface is dislocated towards medially with its posterior fracture line functioning as a hinge. After a simple fall, the femoral head brakes and rotates the anterior column and the quadrilateral surface in opposite directions.
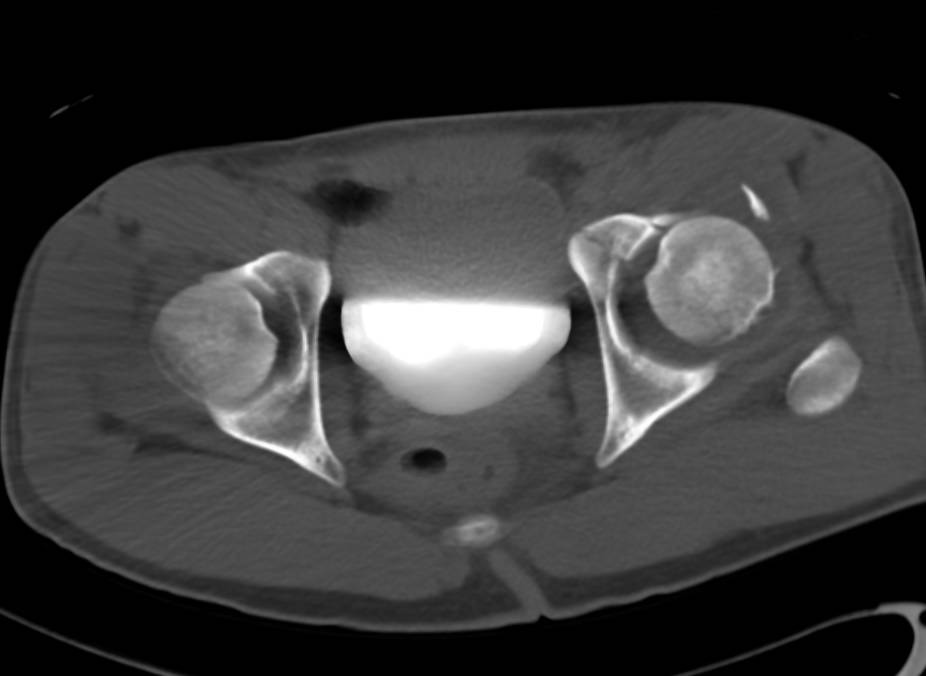
In geriatric acetabular fractures, subchondral impaction and fracture types involving the anterior column and the quadrilateral surface are frequent. Older persons have a reduced bone quality and more often suffer low-energy trauma. The number of acetabular fractures in the elderly meanwhile overtops the number in younger persons. The quadrilateral surface has come under increased attention due to the specific patterns of geriatric acetabular fractures. Additional to the anterior and posterior column, the authors described the quadrilateral surface, which forms the inner wall of the acetabulum and is the lateral wall on both sides of the small pelvis. The column concept, which forms the basis of a universally accepted classification of acetabular fractures, has been introduced by Judet et al in the 1960’s. SF-8 mental remained unchanged.Īcetabular fractures are complex and incapacitating injuries. Quality of life, activity level and mobility importantly dropped as well in this group. In none of these patients, secondary surgery was necessary. 5 of 6 patients (83.3%) could be evaluated after a median of 136 weeks. The concept of medial buttressing was successful in all patients. 50% of patients suffered from in-hospital complications. The median length of in-hospital stay was 18.5 days. The median age of patients of group 2 was 79.5 years, all of them presented with one or several comorbidities. Quality of life, activity level and mobility dropped importantly and were lower than the values of a German reference population. Among surviving patients, 79.2% were evaluated after 3 years of follow-up. Secondary THA was performed in 5 additional patients (5/37 = 13.5%) within the observation period.

ORIF together with primary total hip arthroplasty (THA) was carried out as a single stage procedure in 3 patients. The concept of medial buttressing was successful in all but one patient. 57.5% of patients suffered from in-hospital complications. Their median length of in-hospital stay was 20.5 days. Among them, 82.5% presented with comorbidities. The median age of patients of group 1 was 78 years. Forty patients were included group 1 and six patients in group 2. Forty-six patients were included in this study, 30 males (65.2%) and 16 females (34.8%).


 0 kommentar(er)
0 kommentar(er)
